Stay safe. Stay informed.
As of August 10, 2023 the Infection Control/Employee Health staff will no longer be offering Covid-19 vaccines to the public.
The Mississippi Department of Health has ended the program to give the vaccines to the community for free. Covid-19 vaccines are still offered at many pharmacies and doctor's offices so that the community can continue to stay up-to-date on vaccines. We have thoroughly enjoyed providing the vaccine to help protect our community from an epidemic.
COVID Vaccine Clinic
Every other Friday, 8 a.m. - noon
OCH Community Room
No appointment needed
People age 50 and older can receive a Moderna 2nd Booster and will not require a physician's order.
Click below to learn more about the Moderna vaccine.
This is a new virus and a new vaccine. We understand there are many questions, and we are here to ensure you have accurate, up-to-date information to help you make an informed decision for you and your family.
Click here for answers to frequently asked questions.
Vaccination for 5 - 11 year-olds
Vaccination for pre-teens and teens
Fact Sheets for COVID Vaccines
July Inpatient COVID Statistics
August Inpatient COVID Statistics
September Inpatient COVID Statistics
October Inpatient COVID Statistics
November Inpatient COVID Statistics
December Inpatient COVID Statistics
2021
January Inpatient COVID Statistics
February Inpatient COVID Statistics
March Inpatient COVID Statistics
April Inpatient COVID Statistics
May Inpatient COVID Statistics
June Inpatient COVID Statistics
July Inpatient COVID Statistics
August COVID Inpatient Statistics
September COVID Inpatient Statistics
October COVID Inpatient Statistics
November COVID Inpatient Statistics
December COVID Inpatient Statistics
2022
January Inpatient COVID Statistics
February Inpatient COVID Statistics
March Inpatient COVID Statistics
April Inpatient COVID Statistics
May Inpatient COVID Statistics
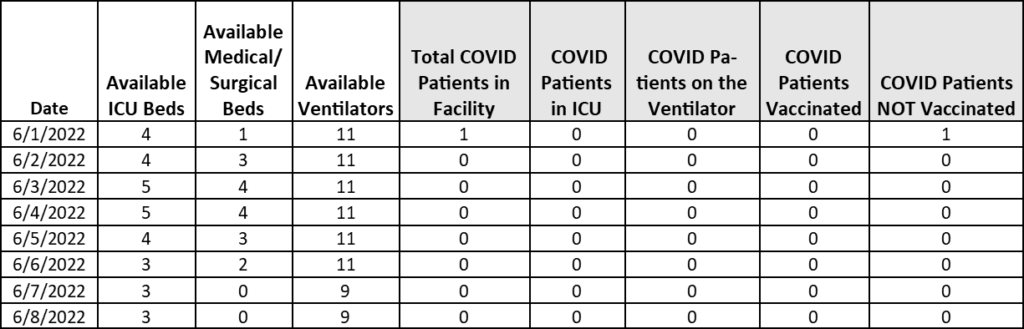
OCH REGIONAL MEDICAL CENTER VISITATION POLICY
OCH continues to be committed to the safety of our staff, patients and visitors. We are guided by the current CDC transmission risk levels to determine whether masks will be required. Please note this policy is subject to change at any time based on transmission rates. This policy goes into effect Monday, March 21, 2022.
- General Acute Care Inpatients: Patient may have two visitors at a time. Visitors may switch out as desired but only two at a time can be in the room. Patients at end-of-life may have more than two visitors if the physician approves.
- COVID-19 Suspect/Confirmed Patients: Patients may not have any visitors unless it is an end-of-life situation. Patients at end of life may have 2 visitors but these visitors may not change throughout the visit.
- Labor & Delivery/Postpartum: Patients may have two visitors at a time. Visitors may switch out as desired but only two at a time can be in the room.
- Pediatric: Visitation may consist of one parent/guardian and one other adult support person.
- Newborn Followup: One parent/guardian and one other designated adult will be allowed to escort the newborn to the followup appointment.
- Outpatient: Adult outpatients may have one visitor throughout outpatient stay. Pediatric patients may have one parent/guardian and one other adult visitor.
- ICU: Visitation will be from 10-10:30AM, 1-1:30pm and 5:00-5:30pm. Two visitors will be allowed into the room at a time during each visitation period. Once a visitor arrives to the ICU waiting room, they should call 2771 or 2772 from the waiting room phone to notify the nursing staff of arrival.
- Emergency Room: Adult patients may have one designated visitor. Pediatric patients may have two adult visitors. COVID ER patients will not be allowed visitors.
- Cafeteria: The cafeteria is open to the general public.
- Medical Records: Medical records is open to the general public.
- Children are allowed in the building but must be accompanied by an adult.
- Wellness Center: Masks are suggested but are not required.
- Cardiac Rehab: Masks are suggested but are not required.
- Outpatient Physical Therapy: Masks are suggested but are not required.
- Clergy: Clergy will be allowed in the building to visit patients. If they are visiting a COVID patient, they must be willing to wear appropriate PPE.
- All OCH Clinics: Masks are suggested but are not required.
- Congregation of visitors is not allowed in OCH waiting rooms.
- Business Office is open for paying bills only. We strongly encourage patients to utilize our online services at och.org and click on “Pay a Bill” or “Visit Patient Portal” on the homepage. To register, call 662-615-2683. If you would like to pay a bill over the phone using a credit card, call the number on your bill or our business office at 662-615-2600 or 662-615-2601.
• Patients and visitors who enter the hospital will no longer have to be screened. In accordance with the current CDC transmission risk levels, OCH will post the level each week for staff and visitors with the required mask requirements.
• This policy does not apply to OCH employees and vendors who have received an exemption with accommodations for the CMS vaccine mandate.
The parking garage is open to the public.
Entrance to the hospital:
1. Outpatient (5 AM-5PM Monday-Friday)
2. West Tower Main Entrance (7AM-7PM 7 days a week)
3. Emergency Department (open 24/7)
4. Parking Garage (open 7AM-7PM 7 days a week)
If you are sick with Coronavirus/COVID-19 or suspect you are infected with the virus that causes COVID-19, follow these steps to help prevent the disease from spreading to people in your home and community.
